A detailed report of an in-hospital EEG study
I chronicled my in-hospital EEG study to share with other TBI survivors and anyone with seizures. My experience will hopefully provide an idea of what it's like, what to expect, and some tips to survive the experience.

Day 1 – August 23, 2021
I was scheduled to arrive at 7:30 AM to check into Swedish Medical Center for my long-anticipated video EEG (electroencephalogram) in-hospital testing. The program is scheduled for five to seven days. Mental preparations are as taxing as the physical preparations. A few months ago, when I spoke to the nurse and scheduled this event, she gave me the low down on what to expect and I asked a lot of questions and jotted those answers down in my notebook. Last week, I referred to my notes to start to “mentally prepare”. I then had additional questions so called the nurse again and to confirm my stay as I had not received any communication or reminders whatsoever, which I think odd given that I’m a brain injury survivor and we are prone to memory issues. That aside, the nurse phoned me back and said I was on her list to call that day and I happen to beat her to it. Geatha answered my questions and again explained to me what to expect. I proceeded to begin packing. Geatha told me there was a lot of “down time” and to bring things to keep me busy. I thought of my never-ending to-do list and chuckled silently.
Bell service hospital style
Yesterday I realized I was going to need help getting all of my things to my room and even though I creatively coined this stay “Club Med” with a humongous pun, I knew there wouldn’t be a luggage cart to lug my “keep me busy” stuff in plus Lucy and her things. I asked a friend to meet me, and we loaded up a wheelchair and ourselves with all my things. We were loaded down for sure. Working from home for twenty years, I have a portable office down. I brought the essentials for equipment and plenty of work, as well as personal business.
Focus on the purpose
An interesting fact about me is I am very routine driven and focused on getting the task completed. This is an excellent trait especially when the task is stressful or could conjure stress. I feel it’s also connected to adrenaline. Whereas I hear a lot of people talk about anxiety and feeling anxious in anticipation of something unknown or stressful, I do not have any of that. Even before I practiced mindfulness intentionally, my brain is predisposed to focus on the matter at hand. On my drive to the hospital, I stopped to treat myself to a decadent latte—something I never do. My coffee drink of choice is a pure decaf Americano. Laugh all you want—I love the taste of coffee but do not like caffeine and gave caffeine up as a teenager. For those of you who know me, I tell people me not drinking caffeine is a public service to those I encounter. Jokingly I ask, “Do you really want to see me on caffeine?”. My positive attitude and abundance of energy would easily lead to hyperactive states, so I avoid Jena on caffeine or any other stimulants. Back to my original point: because I am driven to the task at hand, I don’t feel the emotions of the stressful situation until it’s imminent or I encounter it. That’s what happened this morning as I made my final turn onto the street the hospital is located. As a treat, I decided to pick up a coffee and Caribou Coffee was right on the way. I popped in and ordered a special treat: a malted mocha with dark chocolate and whipped cream. That sounded like a special treat indeed before checking into a hospital “incarceration”.
Reality sets in
That’s when the adrenaline wore off and I was faced with the reality of what was in store for the next five to seven days. I began to feel a mixture of emotions including sadness, loneliness, and a little bit of fear. Keep in mind, the sole purpose of this hospitalization and testing is to get a clearer understanding of the seizures I have from time to time and create a plan to address managing them. I’m willingly driving myself to an extended stay at the hospital to study my brain activity. Yet, the emotional side of me finally surfaced now that the logistics were all handled. Now, it was time for me to feel the emotions of what this two-minute drive from the coffee shop was going to bring. As I parked the car in front of the coffee shop, the emotions started to build from a spark. Immediately upon ordering, with no more logistics to focus on, the spark turned into a roar inside me rising quickly to the point where tears welled in my eyes as I waited for my malted mocha treat. I sent a text to someone who knows this side of me well, looking for comfort, reassurance, and even a sense of belonging. I fought back tears at Caribou Coffee and the barista called my name. I smiled, said thank you, and poured my coffee into my Yeti mug and put on my armor to brace for the final two minutes to my destination.
At this point, I knew I was in a fragile state so sent a text to my friend to please not tease me for all the stuff I was taking, that I was feeling the stress of this, and not strong enough to handle teasing. I needed gentleness, caring, and compassion.
The point of no return
My friend met me at the hospital to help me schlep my things inside. I thought of this idea the day before knowing this was a hospital not a hotel there would not be a bellhop or a luggage cart. I pulled into valet and focused on the task at hand which helped me stay in the moment and not get carried away with the emotions. We loaded up a wheelchair and ourselves with Lucy in tow and walked into the hospital.
I checked in as a direct admit and after a short wait, the registrar sent me on my way to the neuro floor where I would set up camp for the week. Upon walking onto the neuro floor, a smattering of hospital rooms greeted us. It felt like we were in the wrong place or trespassing or something “wrong”. We kept walking and finally I saw someone and told him I was checking in and he guided us down the hall further where we did find a nurses station where they were expecting me. My assigned room is right in front of the nurse station.

The torture begins
The staff entered my room like a parade—one appearing on the heels of another. Many months ago, I had a 72-hour ambulatory EEG so had to come here to have the leads put on my head, so I knew what that process entailed but I had forgotten the stench of the glue and how much tape is used to keep leads in place on the side of my face and forehead where they don’t use the glue. From 7:35 AM to 12:40 PM, I was inundated with staff and getting connected to the equipment.
Then suddenly, I found myself alone with alarms on my hospital bed and my recliner. Not only am I chained from 27 points on my head to a piece of equipment on the wall, but I am also unable to even stand up and stretch without the alarm alerting everyone nearby and the nurse’s station I am up. As a strong, independent, and self-sufficient and very woman, and someone who is used to helping others, not being able to cross the room for something or even stand up to stretch, this may be the most difficult aspect of the testing process. This goes for the bathroom visits too—some nurses are flexible with the policy and stand outside with the door left slightly ajar so I may have some sort of privacy in the bathroom. This major detail was not a topic of discussion with Geatha in either of my conversations with her and certainly when I asked her to describe the setup. Geatha told me I would be able to “roam about the room” but would be tethered to the machine. I knew going into this I wouldn’t even be able to go outside let alone leave my hospital room because the EEG cord doesn’t go that far but I was not advised about being bedridden or chair ridden so this was a huge shock and mental adjustment.
The room
However grossly misrepresented the alarm system and 100% supervised was, the room is as described: a small table with two chairs; a couch; recliner, cubbies, and of course the bed and bathroom. The nurse instructed me to start settling in and so I did. I put down a sheet under Lucy’s bed because it’s a hospital floor—yuck! Then slowly started to acclimate to the new surroundings.
Quickly, the staff barraged me with different things adorning me with the obligatory bracelet, EKG leads, and then the crown, oops, I mean the EEG leads. The EEG process takes about two hours to complete. I was lying comfortably on the bed and Lucy quickly got into nap position since I was in bed. The cacophony of activity suddenly plateaued and I then realized it was 1 PM and no one mentioned the other details of my stay including how to operate the call control, the meal process, and didn’t give me the low down on the room, phone, etc. I went from being bombarded with staff and attention to the complete opposite all while digesting the fact that I was 100% dependent on them for everything in order to be compliant.
Once I was settled in, by the time the shift change at 7 PM occurred, my day nurse Malik explained to the night nurse Rachael I was acclimating to the dependent situation and other than getting hooked up to my newly acquired CPAP machine, there were no other out of the ordinary conditions to comply with or work around. I was free to sleep whenever I chose. I opted for bed at 10:30 after an episode of “Manifest”. I started to twitch last night and wasn’t sure if it was a seizure or not so didn’t push the button to mark the incident on the EEG. I was confused because I also was falling asleep, and one “twitch” may have been a muscle spasm in my leg. I also wanted to see if it showed up on the EEG and they were going to tell me about it. I was so tired I really didn’t want the whole team in here watching to see if it was a seizure or not…that’s a lot of pressure.
Then the respiratory therapist (RT) came in at 10:45 to set up their own CPAP machine because it had “alarms” on it so we couldn’t use my new one. By then, the twitching was long over, and I was in and out of sleep. By the time she was finished and recruiting help because my piece didn’t attach properly, I was no longer sleepy and struggled to fall asleep. The nose piece and headgear were foreign on my head along with the EEG leads. Finally, I fell asleep. Then was awake at 1:30 and 3:30 with the RT and then a nightmare at 4 AM. I did manage to fall back asleep but my first night there was a short night—a rough start to a five- to seven-day study with intentional sleep deprivation on tap.
Day 2 – Tuesday, August 24, 2021
I woke up at 5:30 am but did not want to get up and start the day so dang early knowing today was the beginning of my sleep deprivation day. I couldn’t fathom the idea of sitting in the recliner with my sore glutes and hips screaming all day long (I recently was diagnosed with a torn left hip labrum, so the pain was intense and all muscles around the hips were on fire all the time and was awaiting surgery). I took the CPAP headgear off and of course, the alarms go off and a nurse magically appears.
I wasn’t able to do the virtual stretching class today with Sophie due to the confinement to the bed or the chair, and that was disappointing as my body certainly needs the stretch and movement. My day nurse today was Kat and she and I connected despite her being only 23 years old. Kat came in often to visit with me and gave me some time to stand, stretch, and walk around. Kat enjoyed our conversations and the calm in my room, and Lucy is a hit with everyone.
Sleep deprivation tactics ordered
When Dr. Doshi and the neuro team came in on rounds, he explained to me I had two epileptic activities on the left side of my brain behind my ear. Dr. Doshi told me they were noticeably short lasting just milliseconds. Dr. Doshi ordered the sleep deprivation tactics because they want to see me having a seizure and record it. They confirmed the twitching last night was not a seizure. Dr. Doshi said the two events would not have produced any symptoms had I been awake, and he explained most patients have epileptic events during sleep.
As an active person, this in-person multi-day EEG testing period is difficult because of the mandatory requirement to be on bed or chair alarm. Due to the legal issues surrounding provoking a seizure and the increased chances of injury, they require the bed and chair alarms. In addition to this major shift, my body is severely injured. I have a torn left hip labrum and as a result, my right side is compensating and severely injured also. I have avoided sitting the last two months whenever possible and now all I’m doing is sitting. Last night at least I could lie down in bed and not have so much pain. I could lie down in the bed now but I’m resisting because I will want to sleep, and I am in sleep deprivation mode now until 4 AM. Then I am only allowed to sleep until 8 AM and unable to return to sleep until 9 PM Thursday (the next day) to create a sleep deprivation situation.
My right glute is causing excruciating pain. Sitting is not just inconvenient and a 180-degree shift from my usual level of activity but it’s also causing additional pain making the sedentary lifestyle extremely difficult. Now, we are adding on the sleep deprivation and that is not good. I know the information we gather during this testing time will be so helpful. Short-term pain for long-term gain. I will be so glad to be able to move freely again, sleep at home uninterrupted, and start using my own CPAP machine so I can start the 30-day mandatory use program and then prepare for the hip surgery that is a month from yesterday.
EEG crown itch
Today the itching scalp set in. Tonight, as I force myself to stay awake, I am feeling much itchiness. I’m tired and my eyelids are extremely heavy. Lilly is my night nurse tonight as Rachael didn’t draw my room I guess. I have no idea how she is going to keep me awake until 4 AM Wednesday because I’m ready for sleep right now. I have the obnoxious canned lights on in the other part of the room. I’m writing in the dark here in the corner in the recliner, but I just can’t tolerate the fluorescent lights. They are too bright for someone like me with a brain injury and light sensitivity.
When the nurses come in for vitals or dispense my medication, they immediately release the alarm and I’m able to stand up and stretch. Lilly has one more patient to see and said she will come back to my room and do her charting work so I can walk around or stretch, etc. I love this specialized treatment.
Day 3 – Wednesday, August 25
Forced to stay up until 4 AM, I kept myself busy on my computer and when I was too tired to think, I watched “Manifest” and I don’t even remember what I watched after that, perhaps “Grace and Frankie”, and I fell asleep and woke up at 3:45 AM so I buzzed the nurse so I could get ready for bed and my precious four hours of sleep. Dr. Doshi told me I would have uninterrupted sleep from 4 – 8 AM. I was so excited for those four hours of sleep!
At 5:30 AM, someone entered my dark room. I checked my watch and was cranky when I saw that it was 5:30 AM. The woman announced she was here to draw my blood. I couldn’t believe it! I told her I was told I could sleep 4-8 AM without interruptions and she said she could go away and come back who knows when. I decided to give her my left hand and I slept through it. I do remember I was not my best self and presented a very cranky, sleep-deprived version of me. I didn’t give it a second thought and returned to sleep.
Friends and favors
Paul, my Best Divorced Husband, was due between 7:30 and 8 AM to walk Lucy and bring me a decaf Americano from Starbucks and I knew they would wake me at 8 AM. I woke up a few minutes before 8 and Paul wasn’t there yet, and Lucy still was sleeping. Then the nurses came in and made sure I was awake. Shortly thereafter Paul arrived, and he took Lucy outside. Lucy showed him how to get to the pet relief area. I ate my breakfast and began the anticipation of the “torture” scheduled for the day. Paul took off for his golf tournament and I sat down atop my pile of strategically placed pillows to work through some of my emails and to-do list.
By lunchtime, there was still no word on the “torture”, so I ordered lunch. Just as my lunch arrived, the EEG tech came in with the strobe light to begin the test and I asked her to come after I ate. My friend Sharon called in advance of her scheduled visit, and I remember the tech telling me the test will take ten minutes. I mistakenly told Sharon I would call her back. What I should have told her is to come whenever she wanted as I may not be able to respond to her text or calls if I had a seizure. But no, I didn’t. (Lesson learned for anyone else preparing for this study.)
The real torture begins
I withstood the variety of different light combinations and verbal cues. Just as the tech began the hyperventilation breathing technique, I started to twitch, and a seizure ensued. Immediately, there was a group of nursing staff present. I observed one gal leading the charge and asking me questions. I was unable to speak. I remember blankly looking at the people in the room and observing what was going on around me like I was out of my body and not really present. There was a barrage of questions, for which I had no answers as I was unable to speak and felt removed from the situation. One nurse was writing things on the whiteboard in the room. Others were calling out signs they saw. When it was over, I was completely spent as usual. My limbs become immobile and feel so heavy and detached from my body. My brain tells them to move, but they don’t. They feel like they are filled with cement. Eventually, I was left alone in my hospital bed. I was aware they left me in an uncomfortable position for which I was unable to do anything about it but wait until my brain recovered enough to allow the autonomic systems to come back online. Helpless and motionless, I just lay there patiently waiting as time passed and my brain recovered.
In this post-ictal state, a nurse tech familiar with me and my vivacious personality, unaware of the testing and what happened after the testing, entered my room, and saw me in my non-responsive state. When I didn’t respond to her, she went out for help. The seizure team returned and seemed to double in size—I have no idea if that is accurate because in this state and the seizure state, my awareness and memory is challenged as I am in a catatonic or out-of-body experience during these episodes. Once again they resumed their posts and started barking out comments I later read on the white board including “not responsive to commands”, “unable to move”, and two more things I just can’t recall. The only way we could communicate was with eye blinking. The most important thing I recall from this event is the blank staring with what I imagine must have been big brown eyes darting back and forth between the nurses. I couldn’t even move my head! Eventually they left and left me alone once again in that horribly uncomfortable position. I still was unable to move to adjust the bed myself or ask someone to adjust it for me.
Temporary paralysis fades
Slowly, I started to begin to feel my voluntary systems come back online. First, it’s the fingers in the right hand beginning with the index finger. Then slowly the movement trickles down to the ring finger. Then, the left hand begins to function again in the same order. There was no movement in the legs or toes. Try as I might, I could not wiggle my toes. My legs still were motionless as if they were filled with concrete. When I was able to move, I painfully reached for the buttons to adjust the bed and get me out of that incredibly uncomfortable position. Then, I rested and napped. The neuro team left me alone the rest of that evening and I was permitted to sleep through the night. I took full advantage of it and when my evening visitor and dog walker left shortly after 8:15 PM, I called the nurse and asked to get ready for bed. I was completely wiped out—from the seizure and sleep deprivation.
Day 4 – Thursday, August 26, 2021
I awoke early before sunrise. I fell back asleep and woke again before sunrise and called the nurse. When she came in, I requested she raise my shade and bring me some decaf coffee. I laid in bed watching the sun rise sipping some black decaf coffee—a simple pleasure I love and one thing I could easily enjoy and appreciate while I was confined to the bed and my room. Mornings are quiet and peaceful.

Dr. Doshi and his team came in to see me during rounds and he told me they were going to repeat the “torture” again today along the lines of “get the most for your money” concept. I thought I had “done enough” but not. Now, I had the “knowing” of what torture was to come and wondering if I was going to have another seizure and have to go through all that again. Seizures are exhausting! For me, my entire body shuts down and then slowly but surely the voluntary systems come back online, and my vibrancy begins to return. So, in a matter of a few seconds, all of this flashed through my brain, and I agreed with the team and accepted the plan for the day. The one thing with this type of activity, they don’t tell you when they are going to do it. I decided I would order my lunch earlier than the day before so I would at least have my lunch in my belly before the seizure, if I had one.
Productive time waiting
I busied myself with work so I could be productive instead of watching the clock and waiting and anticipating the torture on tap. Lunch arrived and I appreciated a leisurely lunch as I knew the time was quickly approaching. I really didn’t want to have another seizure but was doing what I needed to do to get the full value of this five-day study. By nature, I’m a positive-outlook oriented individual. I have always been able to do short-term pain for long-term gain, so I dug in my heels and was ready to face whatever transpired for the bigger picture.
Torture time round 2
The torture master arrived shortly after my lunch, and I was smart enough to ask to use the bathroom. Since I was still on an alarm and labeled a “fall risk” I had to have assistance. I’ve never soiled myself during a seizure and am grateful for that because seizures are hard enough as it is. I decided today to empty the bladder so would hopefully not have a first-time bladder release if I did have a seizure. TIP: I highly recommend you do this before your torture begins.
When we were finally ready to begin, she started with the special blinking light tactic. The woman would give me commands such as “close your eyes” and wait a few seconds, and then “open them”. Then she would change the light pattern and repeat those same commands as well as “Open left eye” and then “open right eye only”. The light patterns would change in relation to intensity, frequency, type of blinking light, speed of blinking light, etc. This day I did not have a seizure after the light test, but it left me exhausted and nauseated. I felt like I would vomit.
The test wasn’t over yet though. We immediately went into breathing techniques, which get you to hyperventilate. I found it hard and distressing to hyperventilate. I had to focus extremely hard to follow the directions and it was physically hard for me to breathe that way as a yogi—counterintuitive. The torture master’s behind-the-scenes partner aborted the session and announced, “End the session”. The behind-the-scenes partner was watching the EEG during the entire testing period just as the day before. Although I didn’t have a seizure, I was exhausted and still had nausea from the light test. Just as fast as the test began, it ended, and the torture master wheeled her light away in a flash. I then was free to relax. Later the resident doc came in after my nap and recovery period and announced there would be no more testing and I was free to relax. I was still connected to the alarms so still had to have assistance and bathroom presence but at least the torture was over.
Day 5 – Friday, August 27, 2021
Last night I slept well and ready for discharge! I awoke exceedingly early after an incredibly early bedtime. I rang the nurse for a cup of black decaf and to open the blinds so I could watch the sun rise again. I sat in silence and in gratitude as the sun slowly rose over the horizon and over buildings. I love watching the day begin and things come to life.
Results
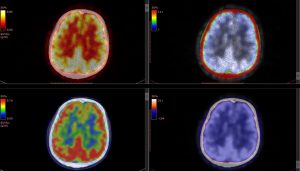
They are discharging me later this morning after five days being bedridden or chair ridden with alarms and being tethered to equipment on the wall which prevented me from leaving my room, with 27 leads affixed to my head, and five EKG leads also attached to my body. The photo stimulation and hyperventilation tactics as well as the five days on EEG 24/7 produced results to further steer my TBI recovery and manage my condition optimally. This study shows there is cause for a PET scan to determine which part of the brain isn’t functioning properly. I have my vote on what’s not working right but the doc wants to be “for sure, for sure” as I like to quote from one of the few jokes I can tell. The PET scan is done as an outpatient process and will do that within the coming months.
I’m excited to go home today and resume my independence and my active lifestyle once again. I’m thankful to my rock star friends who came to visit and take Lucy out for her business so she could stay with me the entire time. This was a very tough week but as usual, I did it Jena-style with positive attitude and grace. Club Med ends today!! Hurrah!!! In three weeks though I have hip surgery, so I am going to enjoy being able to play tennis and move around freely the next three weeks!
Summary for seizure sufferers and TBI survivors
If you suffer from seizures, I encourage you to do the in-hospital testing and monitoring. They really can do much more than an ambulatory EEG (which I had within the year) which prompted further testing. The ability for frequent, comprehensive care with the neuro team with sometimes instant feedback I found rewarding and helpful. It also helped me recharge my determination to finish the study. I appreciated the 24/7 EEG monitoring as it proved to the neurologist there is a hardware malfunction in the brain which my previous neurologist/epileptologist denied. Be your own and best advocate. If you aren’t getting what you want with your team, find a new team. I had to fire my second neurologist I inherited after my initial neurologist retired. The second neurologist nearly caused undue stress and as we brain injury survivors know, stress if the worst enemy for our brains!
In summary, the Club Med experience is worthwhile, but it is a long week. My care team was amazed at how many visitors I had (sometimes three in one day on a good day) and I had no idea how much I was going to need to see those beautiful faces and their gifts of coffee, chocolate, pizza, etc. If epilepsy monitoring makes sense for your situation, I recommend you go in with the expectation of being chained to the bed or a chair, not moving around freely, being monitored 24/7, and be patient.Pack enough to keep your mind occupied in a healthy fashion. Bring your work, your homework, a laptop, a traditional notebook for journaling, puzzles, and coloring kits.
I’m a patient person by training and life’s challenges so I dealt with it well. Even so, it is a HARD week on emotional, mental, and physical levels. I hope the chronicle of my experience helps set the stage for your EMU experience. When I walked out Friday around noon, I was on Cloud 9, my feet were floating. I was so HAPPY to be free and felt relieved to have answers to move my care forward in the proper direction. Best wishes to you.
Be well. Live fully. Love big. Practice loving kindness.